Travel Nurses Explain Working in ICU During COVID-19
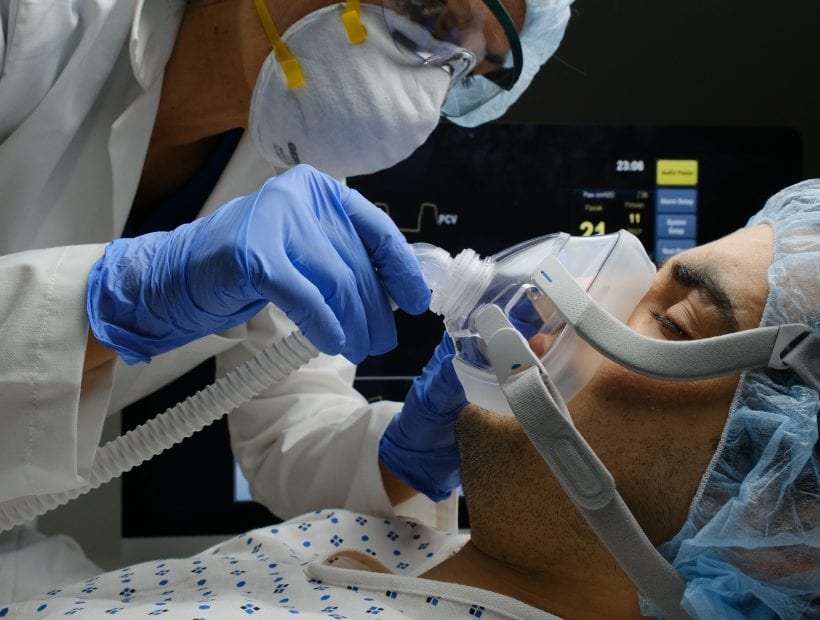
Even during the best of times, ICU nursing is not for the faint-of-heart as these patients require the highest acuity of care. Critical care nursing requires a powerful combination of skills, knowledge, and proactive thinking to sustain life for the most fragile of patients. Whether you’re a new grad nurse or an experienced ICU nurse, working a COVID unit brings a new set of challenges. And we’re breaking them down with insight into what it’s like working during the pandemic on COVID-19 units across the country.
- ICU Nursing During COVID-19: 2 nurses share their experiences caring for patients, from how they’re coping to sedation levels required for vented patients.
- Travel Nursing During a Pandemic: Both nurses report that by remaining flexible and willing, they’re able to continue working.
- Advice for Travel Nurses Working During COVID: It’s important to take care of yourself, and trust that if you’re not working right now, you’re still a valuable nurse.

Part 1: ICU Nursing During COVID-19
Typically, ICU nurses care for patients who are intubated, ventilated, and on life-sustaining medication drips. Working in critical care where life hangs by a thread, nurses must be meticulously organized team players with a deep understanding of disease pathology. Long-term wellness is the name of the game. Now add a novel disease we know little about into the mix. ICU nurses need top-notch critical thinking skills to act quickly and caring hearts to advocate for their patients. Critical care nurses also deal with the severe emotional strain of seeing patients are at their sickest. But they also get to see patients go from near-death to healthy enough to go home. And that’s a cause for celebration.
What is it like critical care nursing in COVID-19 units all over the country? We asked TNAA nurses to tell us about their experiences.

Meet Tiffany, RN BSN CCRN — an ICU travel nurse working in Connecticut on a COVID unit
“My contact is ICU float. I’ve been in the MICU (primarily the COVID19 units) for the past 2.5 months straight. I’m coping pretty well. I’m thankful for social media and technology more than ever during these times. When I’m not at work, I try to get outside for walks, bike rides, etc. My mood is affected by the sun or lack of sun. I’ve found that rainy days are great for streaming shows and movies, reading, and home workouts. I strongly limit my exposure to the media. It makes me so angry most of the time because of the fear tactics, non- compliance, and outright ignorance of people.“
Meet Ben, RN BSN — a travel nurse working in Chicago on multiple units
“These COVID patient’s are really tough to treat. Usually, with acutely decompensating patients, it’s a gradual decline (though sometimes it can be rapid). With COVID patients, when they begin to decline, it’s very rapid. By the time you get lab results (arterial blood gas), and you intervene, the lab results you will send will be worse than the ones you just sent even though you gave more support.
These patients have required the highest levels of sedation I have ever seen a patient receive continuously to maintain compliance with the ventilator; they also need some of the highest ventilatory support I have seen. For example, I had a patient who received 60mg of versed an hour for sedation, and the patient was still waking up and causing dysfunction with the ventilator — making the patient unstable. To give perspective, working in the EP lab, I might give 5mg of versed over 2 hours to keep a patient asleep to tolerate an ablation or a cardiac device being placed into their chest.
The isolation is challenging because it’s a multiple-step process, and it takes time. We are so used to popping in and out of rooms quickly to do tasks. Now, these tasks require thought of what other supplies do I need? Is it time for medication? Do I need to turn? Do I need to send labs? If an emergency comes up, it takes a few minutes to get everything on to get into the room; thus, if a cardiac arrest occurs, it could be a solid minute or two before someone starts chest compressions. That’s a long time for someone to go without oxygen to their brain.“
Part 2: What is it Like Working as a Travel Nurse During the Pandemic?
Our travelers have worked in units all over the country, walking into a new facility every 13 weeks to care for critically ill patients. Before this pandemic, some travel nurses felt that they had to prove themselves to receive tough cases. You can expect that taking a contract now will test your skills and require endurance — think of the influx in elective surgeries as coronavirus cases decline. Despite a traveler’s experience working in new places, walking into a new unit during the COVID-19 outbreak is inherently different.

Tiffany, BSN CCRN
“I started my assignment on March 2, about 2 weeks before stay-at-home orders were issued in CT, and right before we got our first COVID positive patients into the hospital. I was lucky to have already extended for 4 weeks before the real COVID wave here, and have since extended again. It’s tough being a traveler with a secure assignment while I have friends all over who aren’t so lucky.“
Ben, RN BSN
“My original contract put me in the EP lab, but with my experience and skill set, I started working in the ICU. It has been interesting working in two different areas; I will say that working in the EP lab is almost like a break from the constant work of the ICU. Our patients in the EP lab area are usually very thankful for coming to work and helping them out. There is a lot of gratitude, and the overall experience of work makes you feel like you are really helping someone who needs something. Working in the COVID ICU, it is an unknown. It’s unknown if what you are doing will make a difference or if the virus will ultimately win in the long run. It can be hard to do the same thing repeatedly, so working in the EP lab also helps keep my spirits up during this time of crisis.“
Part 3: Advice for Travel Nurses Working During COVID
From busy COVID units to quiet ICUs, travel nursing offers a little bit of everything. Our nurses in northern Maine or Idaho have seen very little of the pandemic. The coronavirus met PACU and OR nurses with cancellations. Meanwhile, in other areas, the pandemic brought pandemonium to nurses working in critical care. Wherever you are now in your travel nurse journey — just starting or waiting to return — your fellow nurses are with you. Know that if you’ve been sidestepped by this virus or find yourself stepping up to fight it in the ICU, you’re not alone.

Tiffany, BSN CCRN
“If you’re a nurse currently looking for an assignment, my biggest advice would probably be to be flexible on location, and if you’re somewhere that you can extend, do that and try to ride it out a bit longer.
I think it’s essential for everyone in every department to remember we are all in this together. Whether you’re directly on the frontlines in the ICUs or med-surg COVID units, or if you’re furloughed for low census — we all have a role.“
Ben, RN BSN
“To my other nurses: Don’t be a hero. You already are, but you have to take care of yourself too because, over time, some of us will get sick, and more work will be required of nurses. It’s a marathon, not a sprint.
For those nurses who might not be working right now because cases are canceled due to COVID, there will come a time when cases come back, and your patients will need you there when they come out of their procedures. You’re probably going to have to work long days and maybe even overtime. Your time will come where you will do your part to make up for the time when COVID was the main focus. You are still a nurse and valuable even when you might not directly be taking care of a coronavirus patient. There is no I in the word team, and it takes lots of people besides the direct bedside nurse to care for those patients. Thus you are valuable and are appreciated.“
Nurse Support & the TNAA Difference
At TNAA, support is at the heart of what we do. We’ve always provided benefits that truly matter, from clinical resources to total well-being and mental health services. And that’s never changing.
Read More: This blog explores the mental health struggles of frontline workers & what resources we’re providing our nurses, from clinical support to mental well-being.







